Traumatic Brain Injury: Expert Q&A
In this expert Q&A, Dr. Michelle Petrak, Ph.D., an audiologist specializing in vestibular testing at Northwest Speech and Hearing in Chicago and the Director of Clinical Research at Interacoustics, and Dr. Gail Whitelaw, Ph.D., audiologist and Director of the Speech-Language-Hearing Clinic at The Ohio State University, discuss traumatic brain injury (TBI), its impact on the auditory and vestibular systems, and how healthcare practitioners can collaborate to diagnose and treat patients. Listen to the podcast or read the condensed Q&A below.
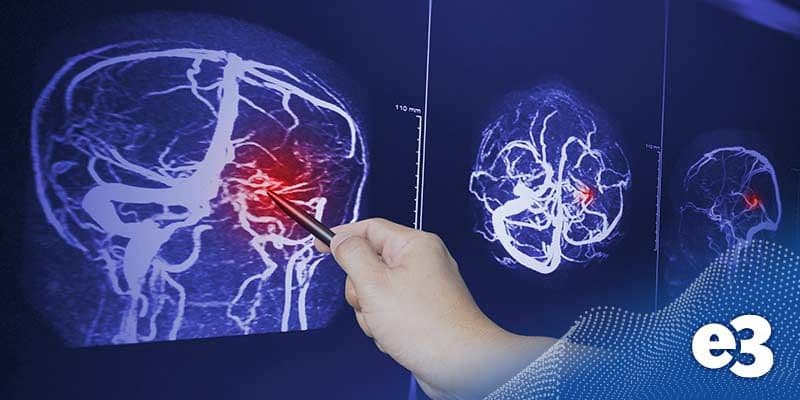
Whitelaw: According to the centers for Disease Control, in a study that was published in 2020, a TBI, or traumatic brain injury is caused by a bump, a blow or a jolt to the head that disrupts the normal function of the brain. A TBI can be classified as mild, which is a brief change in mental status or consciousness.
Petrak: TBIs can result from various incidents, including concussions and sports injuries, combat injuries, car accidents, slips and falls, explosions, and other sports-related injuries.
Petrak: Most of my research focuses on sports-related concussions. In a pilot study with Banner Concussion Center in Phoenix, Arizona, we found that differentiating someone with a concussion from a normal population is quick and easy using an anti-saccade task.
This task involves asking the patient to look away from a presented target, adding a cognitive challenge. Concussed patients struggle with this, making many errors due to ocular motor and cognitive deficiencies. These tests are efficient for diagnosing and monitoring concussions. Additionally, I work with Special Olympics athletes, applying similar methods to assess and treat their injuries.
Petrak: Sure. I worked with a Special Olympics athlete who had difficulties after a fall during practice. Despite a normal checkup by his family doctor, his performance in the standing long jump was below his usual standard.
Vestibular tests showed lower scores compared to his baseline, indicating a concussion. After rehabilitation exercises, his scores returned to baseline, and he regained his normal jump length. This highlights the importance of baseline testing for accurate post-injury assessments.
Whitelaw: TBI can significantly impact auditory processing and communication. Many people with mild TBI receive little care post-incident and may experience post-concussion syndrome, which can last for years. Audiologists play a crucial role in improving functional communication and quality of life for these patients.
Common issues include tinnitus, sound tolerance problems, peripheral hearing loss, and difficulties in noisy environments. For example, I had a patient from the Boston Marathon bombing who struggled with auditory processing and communication upon returning to work, highlighting the long-term effects of TBI.
Whitelaw: Audiologists are essential in the care team for TBI patients. We can address vestibular issues and improve functional communication, providing care that enhances the patient’s quality of life. Our role includes diagnosing and treating tinnitus, sound tolerance issues, and auditory processing problems, ensuring comprehensive care for TBI patients.
Whitelaw: One of my patients, who was in the Boston Marathon bombing, had significant difficulty hearing in background noise and struggled with repeating information. She saw seven audiologists over a year, but none performed a speech-in-noise test, which was her main complaint. She was frustrated and even diagnosed with PTSD by an audiologist, which is outside our scope.
Eventually, she met a colleague who referred her to me. We conducted a QuickSIN and found a significant signal-to-noise ratio hearing loss. This simple test identified her issue, and we provided her with hearing aids and a comprehensive auditory battery. Her quality of life improved dramatically, allowing her to socialize and work effectively again.
Whitelaw: Interprofessional education and practice are crucial in healthcare. Working as a team with physical therapists, neurologists, optometrists, psychologists, and other specialists leads to better patient outcomes. For example, physical therapists can help TBI patients regain driving skills using simulators. This interdisciplinary approach provides comprehensive care and supports the patient’s recovery journey.
Petrak: Absolutely. In our practice, we’ve expanded our team to include optometrists, occupational therapists, and family members, in addition to traditional physical therapy and audiology.
This multidisciplinary approach ensures a complete diagnosis and personalized recovery plan for each patient. We’ve also started incorporating speech-in-noise testing as a routine part of our assessments, which has been very beneficial.
Interested in learning more about vestibular assessments? Our balance specialists are here to help. For more information, please contact your local office.
Need balance equipment? e3 Diagnostics offers top-notch vestibular test solutions from leading manufacturers. With same-day service in many locations, e3 Diagnostics is ready to provide high-quality balance assessment equipment for your ENT practice, audiology clinic, or rehab facility.
Other Good Reads: Starting a Balance Clinic: Your Questions Answered