The differential diagnosis of visual field loss versus visual neglect is often challenging following traumatic brain injury and stroke. Both often result in loss of visual function to one side or hemisphere, more often to left of center, almost as if someone draws a line right down the middle of their vision from top to bottom and then erases one half. Both have severe consequences for the daily living functions of our patients, increasing things like risk of fall and loss of driving privileges. Unlike with concussion, there is often a visible lesion or area of damage that appears on Ct scan or other forms of imaging.
Visual field loss is due to a physiological interruption to the neuro pathways and nerve fibers which leave the eye, traversing their way throughout much of the brain to the occipital lobe. Almost one million nerve fibers exit the eye via the optic nerve on their way to the visual cortex, the nerves from the temporal portion of the eye stay on the same side and the nerves from the nasal portion cross over to the opposite side via the optic chiasm. Strokes, aneurysms, infarcts, or trauma almost anywhere in the brain can cause unique areas of peripheral vision loss. Before the widespread use of x-ray, CT, and other imaging, the pattern of peripheral vision loss was commonly used to pinpoint the location of brain that was affected. (See figure below)

Visual neglect is defined as a neuropsychological inattention to the visual stimulation coming from one hemisphere, again it is most often the left side that is affected. This is due to a lesion in the opposite hemisphere of the brain, away from, and not directly affecting the visual pathways. Typically, neglect has been associated with lesions of the right posterior parietal cortex, often the inferior parietal lobe or temporoparietal junction and may be shown on imaging.
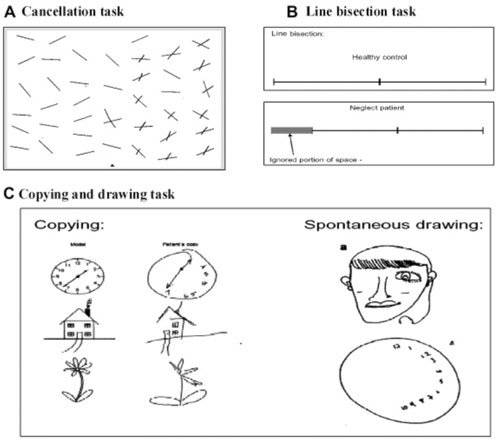
There are many tests to differentiate between neglect and true field loss, some are quite simple and yet very effective, such as the line cancellation test, line intersection test, or having them draw a face or a clock. (See figure below)
Other tests today may be quite sophisticated and require very specialized equipment such as visual evoked response and eye movement registration. Although the differential diagnosis between these two problems is important to help determine the cause and the prognosis, the symptoms, and many of the therapies used to help the patient compensate, adjust, and improve are the same. And, after all, improvement of function for our patients is what is most important to us as clinicians. Remember that visual field loss that has not improved within 3 to 6 months tends to be permanent, with scanning and compensatory therapies needed from that point on. Visual neglect has a much better prognosis, and while compensatory skills are especially helpful and necessary early on, treatments to improve neglect will often aid in recovery and permanent improvements are possible.
The therapy for visual field loss and neglect is often broken down into 2 categories, Top-Down therapy and Bottom-Up therapy. Top-Down therapy is the traditional therapy of teaching the subject to scan into the area of loss or neglect and improving their ability to quickly detect an object, make a saccadic eye movements to position their foveal vision on the target, interpret and process the target information and then scan again to repeat the process. This technique can reduce risk of falls and accidents and add to the quality of life, but some patients with visual neglect do not realize or perceive a problem to an entire hemisphere and therefore are resistant to learn or continue the scanning techniques. The BVT instrument, especially in the Rhythm mode is an excellent device for training these techniques as it randomly places a target in one hemisphere and then the other, requiring the patient to locate then touch that target to get it to “beep” and move back to the other side. The therapy requires them to repeatedly cross the midline, exciting both hemispheres of the brain and re-enforces the task with auditory and motor feedback which of course excites additional areas of the brain. In general, the more areas and modalities that are stimulated, the more effective and the better retained is the therapeutic effect.
Two of the most effective bottom-up therapies are prism adaptation techniques and opto-kinetic stimulations, both of which are easily and effectively performed with the BVT instrument. Since many visual neglect patients do not even recognize that they are ignoring an entire hemisphere (anosognosia), these bottom-up types of therapies tend to be more effective, and their effects tend to persist longer.
Prism adaptation therapy is a technique where large amounts (20+ diopters) of yoked prisms are placed in front of the patient, and the patient then must readjust their spatial orientation to be able to touch a target on the BVT. The prism is then removed, and the patient needs to readjust their visual-spatial orientation again. These readjustments or adaptations can be very helpful in breaking down the neglect.
OKN stimulation therapy as a patient is doing the various midline therapies described earlier, but then adds an optokinetic stimulus in the background. The slow or pursuit phase should be moving toward the area of neglect, causing the eyes and visual attention to be reflectively drawn into the side of neglect. Additionally, the BVT can control target size and sensitivity as well as the contrast and speed of presentation of the OKN stripes. With the BVT, these two types of bottom-up therapies can be combined at the appropriate stage of therapy.
About the Author:
Charlie Shearer, OD has been a nationally recognized leader in the areas of vision therapy, visually related learning problems and sports vision enhancement. He has worked with US Olympic athletes and teams, professional and amateur athletes, and coordinated national screening of both Special Olympics and Junior Olympics. Charlie is a leader in the field of instrumentation development as related to his role of Vision Science Consultant for Bertec Corporation, as well as his work with other companies. Charlie was born in Mishawaka, Indiana. He received his undergraduate and optometry degrees from Indiana University. When Charlie returned to Mishawaka, he resumed care of the patients of retiring Dr. Lou Fishman. Soon after, Charlie relocated his practice with Jonathan Kintner, OD. Throughout his career, Charlie has had particular interest in pediatric vision, neuro-optometry, vision training and visual perceptual problems. He also has an interest in sports vision and continues to consult with the Colorado Rockies Major League Baseball team.