Overview of Postural Instability in PD for Physical Therapists

Parkinson’s Disease (PD) brings various motor symptoms, one of the most debilitating being postural instability. This blog discusses:
1. What postural instability is.
2. Causes, progression, and impact of postural instability in PD to help physical therapists (PTs) support patients effectively.
3. Assessing postural instability in PD.
4. Physical therapy (PT) treatments for postural instability, including the use of virtual reality (VR).
What is Postural Instability
Postural instability refers to a reduced ability to maintain an upright position and balance, particularly when standing or walking. For many PD patients, this symptom leads to frequent falls, impacting quality of life and increasing the risk of serious injury.
Parkinson’s Disease Postural Instability
In Parkinson’s disease, postural instability manifests as difficulty maintaining balance during movements, often leading to difficulty with gait. This symptom frequently progresses over time, appearing in later stages of PD and worsening with disease progression. Unlike early-stage motor symptoms, such as tremors or rigidity, postural instability can significantly disrupt daily functioning, necessitating targeted interventions to prevent falls and enhance mobility.
What Causes Postural Instability in Parkinson’s Disease
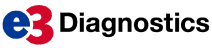
In Parkinson’s disease, postural instability typically results from damage to motor pathways that control balance and muscle coordination. Specifically, Lewy bodies —abnormal aggregates of protein—build up in brain cells, particularly in the areas that regulate movement, contributing to PD progression. Neurotransmitters changes such as dopamine also affect muscle control, balance, and posture.
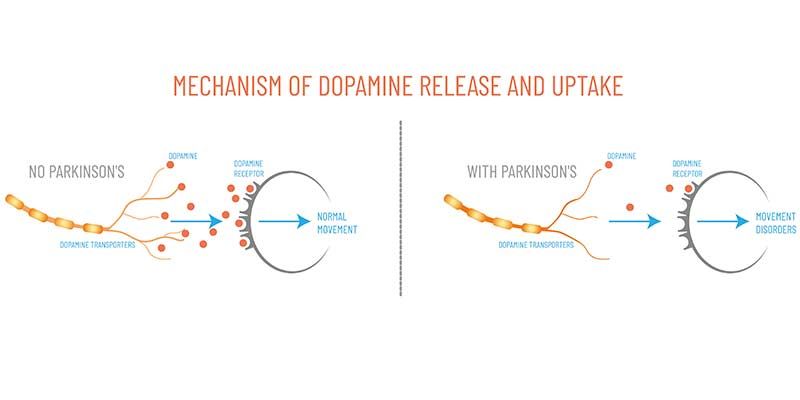
Patients may experience different symptom profiles. Some have tremor-dominant Parkinson’s disease, where tremors are more pronounced than postural instability. Others exhibit postural instability and gait difficulty (PIGD), often indicating a more progressive form of the disease. PIGD patients are more likely to experience frequent falls, cognitive impairment, and mobility issues than those with the tremor-dominant form.
Postural Instability in Parkinson’s Disease Progression
The severity of postural instability in Parkinson’s disease is measured using the Unified Parkinson’s Disease Rating Scale (UPDRS). This clinical tool evaluates motor function, mental state, and activities of daily living in PD patients. A specific part of this scale focuses on postural instability, with higher scores indicating greater impairment. Moreover, PIGD scores categorize PD patients based on their symptom presentation, which is crucial for personalized physiotherapy interventions.
As the disease advances, cognitive impairment may accompany postural instability, making it challenging for patients to compensate for balance issues. Cognitive decline impacts gait and postural control, leading to a greater likelihood of falls and a reduced ability to recover from sudden balance disruptions. This progression underscores the need for an individualized and adaptive approach to treatment.
Postural Instability Assessment in Parkinson’s Disease Patients
Signs of postural instability may include reduced stride length, slower walking speed, or an increased need for support while standing. Physical Therapists can evaluate a patient’s postural stability through clinical balance assessments, such as the Pull Test or the Timed Up and Go Test, to gauge patient’s balance and fall risk.
Postural Instability Physical Therapy Treatment
Given the physical and emotional toll of postural instability, treatment should aim to enhance quality of life and reduce fall risk. Key strategies for PTs include:
Gait Training and Balance Exercises
Gait training in PD aims to restore natural walking patterns with exercises like treadmill walking, which encourages larger strides and faster steps to counteract the characteristic PD gait difficulty. Step-over obstacle courses are also used to train patients to lift their feet and take intentional steps, reducing shuffling and improving stride length.
Balance exercises address postural instability by enhancing core strength and reaction time. Standing on unstable surfaces, like foam pads or balance boards, challenges stability and encourages steady postural control. Weight shifting exercises, where patients lean from side to side or forward and backward, help improve dynamic balance, allowing PD patients to recover more quickly if they stumble.
Strength Training
Strengthening core and lower body muscles can improve stability and reduce fall risk. For PD patients, the primary goal is to develop functional strength that enables them to handle common postural demands, such as rising from a chair or maintaining balance while walking.
Use of Assistive Devices
For advanced PD patients, assistive devices like walkers or canes provide added support, allowing them to move more confidently. Physical therapists can recommend and train patients in using assistive devices to maintain independence while prioritizing safety.
Cognitive-Motor Training
Cognitive impairment in PD patients affects not only memory but also executive function, influencing balance and postural control. Cognitive-motor training involves tasks that require simultaneous cognitive and physical engagement, like walking while counting. Such activities help improve focus, decision-making, and coordination, essential for managing postural instability in PD.
Patient and Caregiver Education
Educating patients and their caregivers on fall prevention and home safety can prevent injuries. Patients can benefit from simple adjustments, such as securing rugs or installing grab bars, to ensure a safe living environment. Additionally, understanding the importance of consistent exercise can motivate patients to maintain their PT routines.
Measuring Progress and Adjusting Treatment
The UPDRS and PIGD scores can help PTs measure a patient’s progress and adjust treatment accordingly. For instance, a high PIGD score may indicate the need for a more intensive focus on postural control and gait training, while patients with high cognitive impairment scores might require more cognitive-motor training.
Tracking progress through regular assessments allows PTs to identify improvements and make necessary adjustments to the treatment plan, ensuring that the therapy remains effective as the disease progresses.
Treating Postural Instability in Parkinson’s Disease with Virtual Reality
Treating Parkinson’s disease (PD) with virtual reality (VR) technology is revolutionizing rehabilitation approaches. VR systems, such as Virtualis, provide immersive environments that engage patients in dynamic and interactive exercises, promoting movement and coordination in a controlled setting.
These virtual simulations can be tailored to address specific symptoms of PD, such as postural instability and gait difficulties, allowing patients to practice functional movements safely. Additionally, VR offers many benefits such as enhances motivation and adherence to therapy. As patients navigate virtual obstacles and scenarios, they can improve their balance, reaction times, and overall mobility, leading to better functional outcomes and improved quality of life.

Virtual reality technology, particularly platforms like Virtualis, is an innovative tool for treating Parkinson’s disease.