Understanding Visual Vertigo: Symptoms, Causes & Treatments

Visual vertigo is a complex condition where patients experience dizziness, disorientation, or unsteadiness triggered by visual stimuli such as moving patterns, crowded environments, or scrolling on screens.
This visual-vestibular mismatch can make daily activities challenging and often requires a tailored approach to treatment. As physical therapists, understanding visual vertigo’s causes, symptoms, and management options can be critical to helping patients regain stability and confidence.
What is Visual Vertigo?
Visual vertigo, or visually induced dizziness, occurs when we rely too heavily on visual input to maintain balance—often due to impaired vestibular function. Under typical conditions, our balance relies on a combination of visual, vestibular, and proprioceptive inputs working in harmony.
For individuals with visual vertigo, heightened sensitivity to visual cues can result in dizziness or discomfort, especially in response to complex patterns, crowded spaces, or rapid movements.
This condition is often linked to visual dependency, where the brain overly depends on visual information for spatial orientation, leading to a sensation known as “space and motion discomfort.” Everyday tasks, like navigating busy stores, can easily trigger feelings of dizziness or instability for those affected.
What Causes Visual Vertigo?
Visual vertigo usually happens when there is a mismatch between what we see and how we feel. This causes the brain to get mixed signals.
This often occurs after a vestibular disorder or head injury. In these cases, the vestibular system affects the patient, making them more reliant on their vision. Common vestibular conditions associated with visual vertigo include:
Benign Paroxysmal Positional Vertigo (BPPV): A common cause of vertigo. BPPV happens when small crystals in the inner ear become loose. This can cause dizziness during certain head movements.
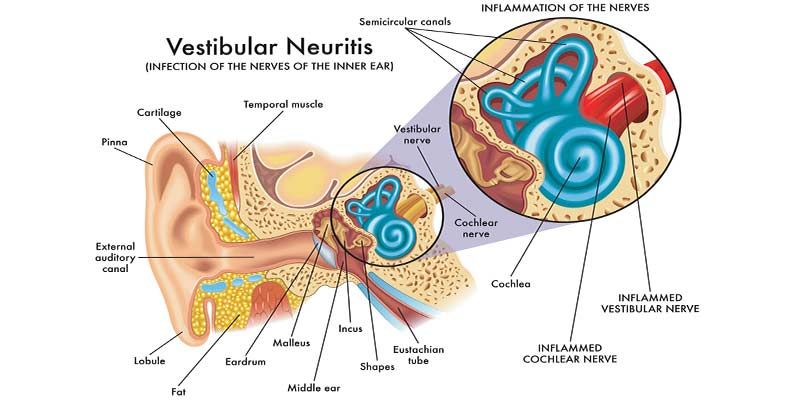
Vestibular Neuritis: Inflammation of the vestibular nerve can create vestibular dysfunction, contributing to a reliance on visual input.
Persistent Postural Perceptual Dizziness (PPPD): Causes ongoing dizziness that can get worse with visual stimuli. This happens even when there are no active vestibular problems.
Symptoms of Visual Vertigo
Visual vertigo can cause symptoms like dizziness, nausea, and confusion. Symptoms are triggered by visual cues like scrolling screens, moving patterns, or bright sunlight.
Symptoms can include:
- Dizziness and lightheadedness; often triggered by busy or moving visuals.
- Disorientation and difficulty navigating crowded or patterned spaces.
- Nausea and motion sickness with repetitive visual stimuli.
- Sensitivity to visual motion.
- Unsteadiness or imbalance in visually stimulating environments.
- Avoidance of places or situations that worsen symptoms.
- Eye strain, fatigue, headaches, and discomfort in visually complex settings.
Will Visual Vertigo Go Away?
Visual vertigo’s duration varies significantly among patients, depending on its cause. For some, symptoms may diminish naturally, especially if linked to temporary vestibular dysfunction like BPPV or vestibular neuritis. However, for those with chronic conditions like PPPD, symptoms may persist if untreated.
The good news is that visual vertigo can be treated. With the right help, many patients feel better and function well.
Physical therapists can play a key role in helping patients manage and reduce their symptoms through exercises that promote sensory integration. Early intervention with vestibular rehabilitation therapy (VRT) is particularly beneficial in achieving long-term symptom management.
Treatments for Visual Vertigo
Treating visual vertigo involves a combination of vestibular rehabilitation therapy, desensitization exercises, and sometimes medication. Here are several effective treatments to consider:
Vestibular Rehabilitation Therapy (VRT): VRT is the mainstay of treatment for visual vertigo and focuses on helping patients adapt to visual-vestibular mismatches. Exercises target balance, eye movement coordination, and head movements to improve sensory integration. A progressive approach to VRT helps patients adapt to difficult visual stimuli. This reduces their reliance on visual input for balance.
Visual Desensitization Exercises: For patients who are sensitive to specific visual triggers, desensitization exercises can be helpful. Gradually exposing patients to environments that trigger symptoms allows the brain to adapt to visual stimuli over time. This technique is especially effective for patients experiencing discomfort in crowded spaces or busy environments.
Medication: In some cases, medication may help support symptom management. Acetazolamide is a new treatment for visual vertigo. It can help reduce dizziness by lowering fluid in the inner ear. This helps to stabilize balance.
Lifestyle Modifications: Simple adjustments can help patients avoid symptom triggers. Advising them to wear sunglasses in bright environments, limit screen time, and take breaks in visually intense spaces can make a significant difference. Additionally, encouraging them to focus on head movement control can help reduce visual dependency.
Cognitive Behavioral Therapy (CBT): Visual vertigo can be mentally taxing, especially when it disrupts daily activities. CBT can help patients cope with the anxiety or frustration they may experience, supporting a more positive and proactive approach to their condition.
Addressing Visual Triggers: Identifying specific visual stimuli that exacerbate symptoms is essential. Collaborate with patients to create an environment that reduces visual strain and helps them manage their symptoms. Occupational therapists may also be able to assist in modifying the patient’s environment.
Virtual Reality (VR) Therapy: VR is an emerging tool for treating visual vertigo by safely exposing patients to environments that trigger their symptoms. VR therapy offers a safe, immersive experience. It helps patients adjust to difficult visual situations. This can improve their resilience and lower symptoms over time.